Approximately 60 percent of adults in America are living with at least one chronic medical condition and 42 percent have two or more chronic conditions.1More than two thirds of all deaths are caused by one or more of the following chronic disease states: heart disease, stroke, diabetes, cancer, and chronic obstructive pulmonary disease.2 Meanwhile, nearly one in five adults live with a mental illness.3
How common are co-occurring disorders?
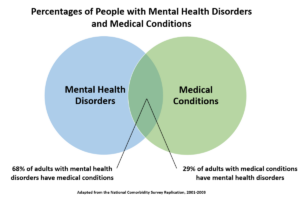
According to the 2001-2003 National Comorbidity Survey Replication (NCS-R), 68 percent of American adults with a mental health disorder reported having at least one general medical disorder, and 29 percent of those with a chronic general medical condition had a comorbid mental health disorder. 4,5
The authors of the 2008 Milliman Research Report sought to analyze the impact of comorbid depression and anxiety on patients with common chronic medical conditions.6
As shown in Figure 1, there is a disconnect between the percentage of individuals with chronic medical conditions that are expected to have depression and the percentage of individuals who are treated for depression. This gap in healthcare is especially concerning because the presence of mental health conditions can adversely impact the treatment of other chronic conditions.
Do comorbidities increase with age?
While the prevalence of U.S. adults with multiple chronic medical conditions has remained steady at around 42 percent, the prevalence of multiple chronic conditions is 81 percent among adults 65 years and older.1 As the global population ages, it is anticipated that the overall number of patients living with comorbidities will increase.8 The increased likelihood of developing multiple chronic medical conditions underlies rising medication use among older adults.
In regards to mental health, it is estimated that 20% of people ages 55 years or older experience some type of mental health concern. Depression is the most prevalent mental health condition among older adults and the rate of older adults with depressive symptoms tends to increase with age. Depressive disorders can adversely affect the course and complicate the treatment of other chronic medical conditions.7
How common is polypharmacy in older adults?
Approximately 44 percent of men and 57 percent of women older than 65 years take five or more nonprescription and/or prescription medications per week. As discussed during Genomind’s webinar titled, Pharmacogenetic Considerations for Treatment of the Geriatric Population, a patient taking 5 to 9 medications has a 50 percent probability of a drug-drug interaction.9
What are the risks of polypharmacy?
Older adults, especially those with multiple chronic conditions, are susceptible to the negative consequences associated with polypharmacy. This includes:9,11
- Greater healthcare costs
- Adverse drug events
- Drug interactions
- Medication non-adherence
- Functional decline
- Geriatric syndromes
- Delirium
- Falls
- Dizziness
- Syncope
- Incontinence
Another challenge that clinicians face when treating patients with comorbid conditions is that many of the commonly prescribed treatments for chronic medical conditions can exacerbate the comorbid mental and/or medical conditions.4 For example, various anticonvulsants, corticosteroids, antihypertensives, and gastrointestinal agents have been linked to symptoms of depression.10
Optimizing drug therapy is an essential part of caring for an older person. Prescription and nonprescription medications need to be used with special caution in the older adult population because of age-related changes in pharmacokinetics, comorbid conditions, drug interactions, and more. Pharmacogenetic (PGx) testing provides additional insight into optimizing drug therapy and can help healthcare providers develop a personalized treatment plan.
An opportunity for personalized medicine
Many of the medications used to treat common chronic medical conditions have PGx guidelines associated with them. For example, the Clinical Pharmacogenetics Implementation Consortium (CPIC) provides clinical guidance to help healthcare providers understand how genetic test results should be used to optimize drug therapy for the following medications:
In order to help clinicians navigate the available pharmacogenetic guidelines, Genomind provides clinicians with access to GenMedPro™, our gene-drug interaction software that includes 95 percent of the most commonly prescribed medications.
GenMedPro™ serves as an outstanding tool to help evaluate both gene-drug and drug-drug interactions, pharmacogenetic guideline recommendations, and alternative medication options, as appropriate. This robust interaction database can help clinicians assess personalized medication options and regimens for their patients. To learn more about GenMedPro™ or to request a demonstration from our PhD and PharmD experts, please utilize Genomind’s Clinician Portal. Not yet registered for an account? Register with Genomind to use our precision tools and services and help your patients get better.
References
- Buttorff C, Teague R, Bauman M. Multiple chronic conditions in the United States. Santa Monica (CA): RAND Corporation; 2017.
- Raghupathi W, Raghupathi V. An Empirical Study of Chronic Diseases in the United States: A Visual Analytics Approach. Int J Environ Res Public Health. 2018;15(3):431. Published 2018 Mar 1.
- U.S. Department of Health and Human Services, National Institutes of Health, National Institute of Mental Health. Mental Health Information. Bethesda, MD.
- Druss BG, Walker ER. Mental disorders and medical comorbidity. Synth Proj Res Synth Rep. 2011;(21):1-26.
- Alegria M, Jackson JS, Kessler RC, Takeuchi D. National Comorbidity Survey Replication (NCS-R), 2001–2003. Ann Arbor: Inter-university Consortium for Political and Social Research, 2003.
- Melek S, Norris D. Chronic Conditions and Comorbid Psychological Disorders. Seattle, WA: Milliman; 2008.
- Centers for Disease Control and Prevention and National Association of Chronic Disease Directors. The State of Mental Health and Aging in America Issue Brief 1: What Do the Data Tell Us? Atlanta, GA: 2008.
- Fiske A, Wetherell JL, and Gatz M. Depression in older adults. Annu Rev Clin Psychology 2009;5:363-389.
- Maher RL, Hanlon J, Hajjar ER. Clinical consequences of polypharmacy in elderly. Expert Opin Drug Saf. 2014;13(1):57-65.
- Qato DM, Ozenberger K, Olfson M. Prevalence of Prescription Medications With Depression as a Potential Adverse Effect Among Adults in the United States. JAMA. 2018;319(22):2289–2298.
- Inouye SK, Studenski S, Tinetti ME, Kuchel GA. Geriatric syndromes: clinical, research, and policy implications of a core geriatric concept. J Am Geriatr Soc. 2007;55(5):780-791. doi:10.1111/j.1532-5415.2007.01156.x