Cost and Coverage
We believe personalized medicine should be a standard of care, which is why part of our mission is to make our genetic testing affordable.
What you can expect to pay for Genomind testing and services
Commercial insurance (US only)
$399 prepayment is required prior to testing.
Genomind coverage varies by insurance plan. You may have to cover a portion of the cost, such as a copay or deductible. Please contact your insurance plan for coverage and estimated cost.
Traditional Medicare (Part B) / Fee-For-Service
You will pay $0 out-of-pocket if coverage criteria are met and the test is ordered by a PECOS-enrolled provider.
Genomind PGx testing is covered nationally by Medicare Part B.
Medicare Advantage (Part C)
$399 prepayment is required prior to testing.
Medicaid and Managed Medicaid plans
You will pay $0 out-of-pocket.
Note: the prior authorization will be requested.
What if you still can’t afford Genomind?
We never want finances to prevent you from accessing safer, individualized treatment. This is why we provide resources to help you navigate payment.
Payment Plans
Genomind has partnered with Affirm, which allows you to split out-of-pocket costs into more-affordable payments. Affirm does require a soft credit check.
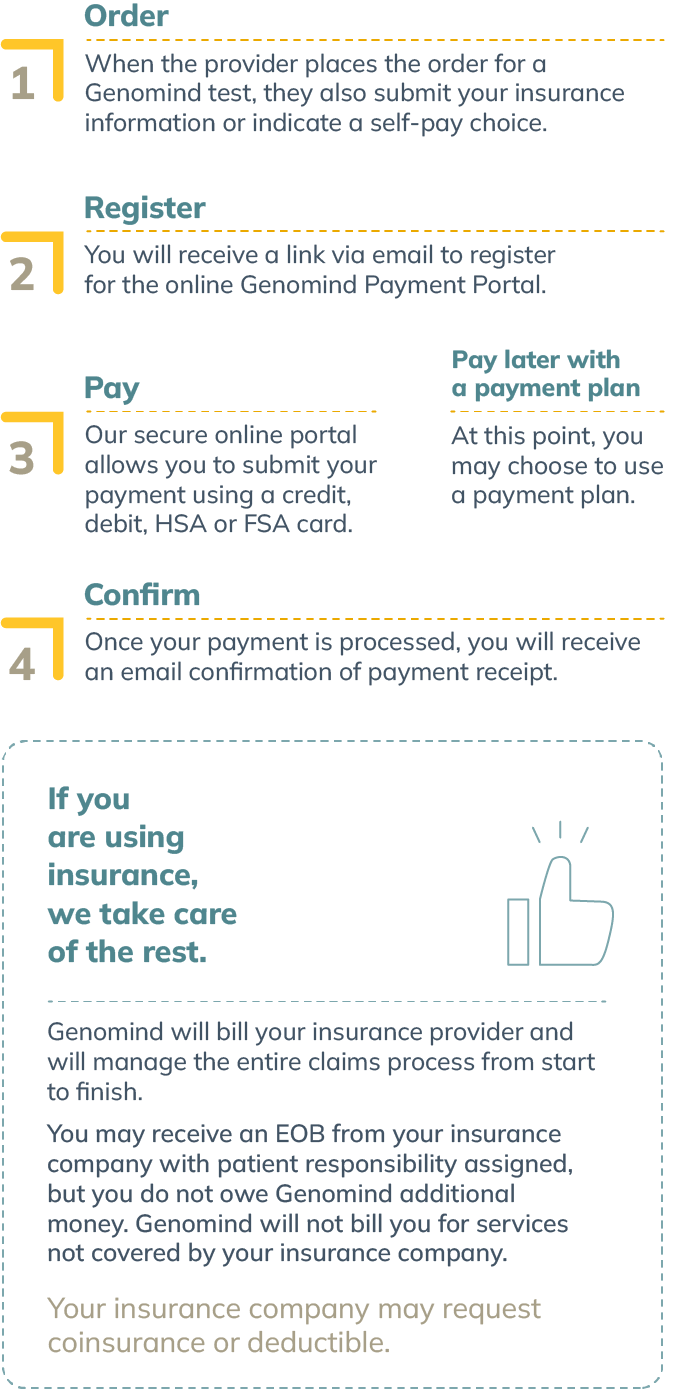
What is the process for payment?
Frequently asked questions (FAQs) about cost and coverage
Genomind is unable to determine specific insurance coverage prior to submitting a claim. Several factors may impact the cost, such as a deductible, out-of-pocket cost, copayment, plan type, diagnosis and medical necessity.
If you are unsure about your coverage or anticipated costs, please contact your insurance plan.
We do not bill you for services not allowed or denied by your insurance plan. If your insurance plan denies coverage, Genomind will file an appeal to pursue coverage on your behalf with your insurance plan. We may need to contact you or your provider during the appeal process for additional information.
Please reference our CPT codes for insurance prior authorization, which also includes our tax ID and NPI number. Contact us if you require additional information.
An Explanation of Benefits (EOB) statement is not a bill from Genomind and is generated by your insurance plan. Each time your insurance company processes a claim submitted by you or your healthcare provider, you will receive an Explanation of Benefits (EOB) statement to explain how your claim was processed. An EOB explains how your benefitscover the service provider’s claim. It includes the date you received the service, the amount billed, the amount covered, the amount your insurance plan paid, the amount credited toward any deductible, and any balance you may be responsible for paying the provider. If you receive an EOB and have questions about it, please contact your insurance provider.
If your insurance plan has reimbursed you directly for our Genomind PGx testing, it is your legal obligation to forward the payment to Genomind for services rendered, along with a copy of the Explanation of Benefits (EOB). It is important to include a copy of the EOB in order to appropriately apply payments to your claim. If your insurance notifies us that you have received payment for Genomind laboratory services, you may receive a bill for the reimbursement you received.
You can forward the insurance payment you received in one of three ways:
- Endorse the check – sign the back of the reimbursement check you received from your insurance, and print “Payable to Genomind” underneath your signature.
If you already cashed the reimbursement check:
- Write a personal check in the amount of the payment you received. Please make the check payable to Genomind.
- Contact our billing team at 844-217-5017 and make a debit or credit card payment over the phone.
Please send your check and EOB to the following:
Attn: Billing Department
Genomind, Inc.
PO Box 74008113
Chicago, IL 60674-8113
If your insurance plan requires prior authorization, we will submit one on behalf of you and your provider. Your provider can request prior authorization prior to submitting your sample.
Even if prior authorization is obtained, you may still be responsible for an out-of-pocket cost.
Yes, inform your provider that you would like to pay for testing instead of utilizing your insurance plan. Your provider will need to select self-pay as your payment method when ordering your test.
Since Genomind’s pharmacogenetic testing report contains information about prescription medication and dosages, the report must be ordered by a prescribing clinician per FDA guidelines. You should not make any changes to any medical care (such as medications, diet, exercise, etc.) without consulting your provider.
We accept all major credit and debit cards, as well as HSA and FSA. Genomind has partnered with Affirm to assist patients with payment options. We do not accept checks or money orders.
Email billing@genomind.com for an itemized receipt of the Genomind PGx testing.
Genomind’s Pharmacogenetic Testing, Precision Medicine Software, and expert Precision Medicine Consultations are available at no cost to providers.
To me, using this service is a no-brainer. It can save time, money, and angst on appointments and medications that aren’t likely to work for you because of the way you’re hard-wired.
Brandon B., Genomind PGx Patient
