Medications with anticholinergic activity have a wide range of physiological effects and are useful in treating a variety of medical conditions that are common in the older adult population. However, older adults are especially susceptible to the adverse effects of anticholinergic medications which can lead to serious physical and mental impairment.1
What Does Anticholinergic Mean?
Anticholinergic is defined as opposing or blocking the physiologic actions of acetylcholine.2 Acetylcholine is a neurotransmitter utilized by both the central and peripheral nervous systems. Anticholinergic medications act as antagonists to reduce or prevent the effects of acetylcholine at nicotinic and/or muscarinic receptor sites.3
What are Anticholinergic Drugs Used to Treat?
Anticholinergic drugs have effects on respiration, circulation, vision, alertness, and more. Drugs with anticholinergic activity are useful for treating several conditions including:3
- Allergies
- Asthma
- Cardiovascular disease
- Chronic obstructive pulmonary disease (COPD)
- Mydriasis
- Parkinson’s disease
- Urge incontinence
While anticholinergic medications are therapeutic for many conditions, countless medications possess anticholinergic properties that are not responsible for their therapeutic effects and increase the risk of adverse events. This includes the antipsychotics, tricyclic antidepressants, diphenhydramine, and more.3
What are the Adverse Effects of Anticholinergic Drugs?
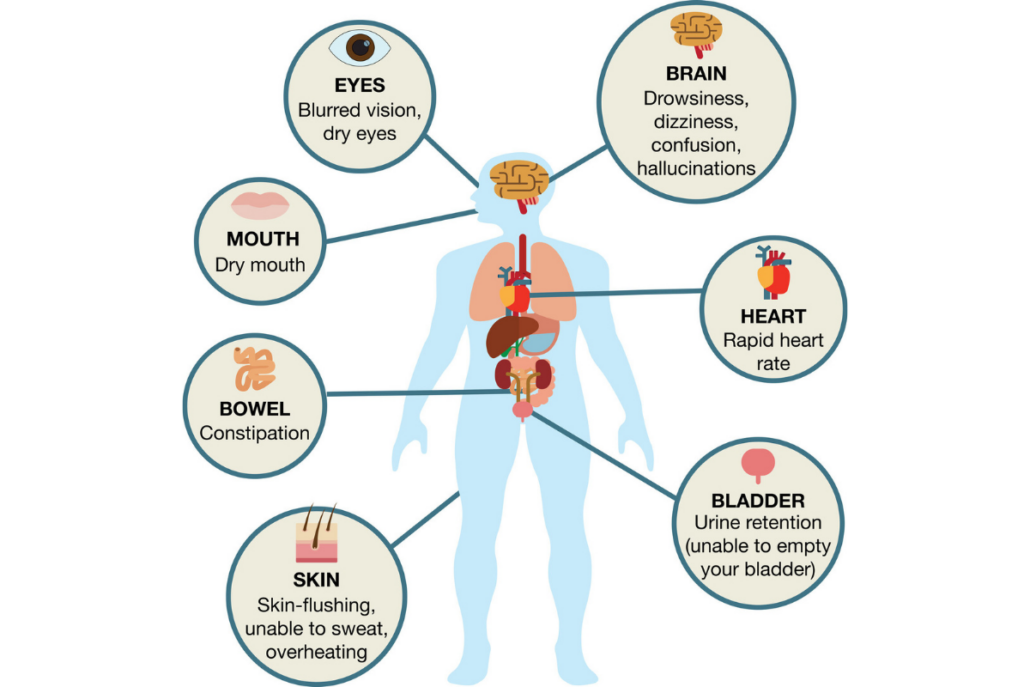
The adverse effects of anticholinergic drugs are divided into central and peripheral effects. Medications that are able to more readily cross the blood-brain barrier have an increased likelihood of causing central adverse effects. Central anticholinergic adverse effects may include:1
- Attention deficit
- Confusion
- Impaired concentration
- Memory impairment
Common peripheral anticholinergic adverse effects may include:1
- Blurred vision
- Constipation
- Decreased sweating
- Dilated pupils
- Dry mouth
- Tachycardia
- Urinary retention
Additionally, many conditions that are common in the older adult population are negatively impacted by anticholinergic medications. This includes dementia, hyperthyroidism, glaucoma, prostate hypertrophy, tachyarrhythmia, and more.3
According to the AGS Beers Criteria®, the main risk rationale for avoiding or minimizing anticholinergic drugs in older adults is due to the increased risk of cognitive decline.4 But how exactly do we know the likelihood of individual drugs and drug combinations for causing these adverse effects and risks?
What is the Anticholinergic Burden?
The anticholinergic burden is the cumulative effect of using multiple drugs with anticholinergic activity together. Dr. Malaz Boustani, a researcher at the Indiana University Center for Aging Research, and her colleagues developed a scale called Anticholinergic Cognitive Burden (ACB) Scale to provide clinicians with practical guidance for using anticholinergic medications in older adults.7
Studies that utilized the ACB scale have demonstrated that higher anticholinergic burden predicts cognitive impairment in older adults.5 According to a recent systematic review that identified 19 anticholinergic burden scales and 104 validation studies, the ACB scale achieved the highest percentage in quality.
The ACB scale categorizes anticholinergic medications on a scale of 0 to 3:8
- ACB score 0 means no anticholinergic effect
- ACB score 1 represents possible anticholinergic effect but no clinically relevant negative cognitive effects
- ACB scores 2 and 3 mean definite anticholinergic effect, with a score of 3 being based on blood-brain barrier permeability and association with the development of delirium
The total added score of different drugs determines the accumulative ACB. Anticholinergic burden should also take into account dosing and potency of medications. If anticholinergic drugs need to be used in older adults, they should be used at the lowest doses for the shortest time possible.
An Opportunity for Personalized Medicine
Prescription and nonprescription medications need to be used with special caution in the older adult population because of the anticholinergic burden, age-related changes in pharmacokinetics, comorbid conditions, drug interactions, and more. Pharmacogenetic (PGx) testing provides additional insight into a patient’s individual drug metabolism profile. This insight can help healthcare providers develop a more patient-specific treatment plan.
For example, consider amitriptyline which has an ACB score of 3. Amitriptyline has specific dosage adjustments for CYP450 poor metabolizers. The FDA Table of Pharmacogenomic Biomarkers in Drug Labeling specifically cites “…poor metabolizers have higher than expected plasma concentrations of tricyclic antidepressants (TCAs) when given usual doses. Depending on the fraction of drug metabolized by CYP2D6, the increase in plasma concentration may be small, or quite large (8 fold increase in plasma AUC of the TCA)”.9
In addition, the Clinical Pharmacogenetics Implementation Consortium (CPIC) provides further dosing recommendations for TCAs based on CYP2D6 and CYP2C19 phenotype. According to the CPIC Guideline, amitriptyline use should be avoided in a 2D6 poor metabolizer but if use is warranted, consider a 50% reduction of the recommended starting dose.10
In order to help clinicians navigate the available pharmacogenetic guidelines, Genomind provides clinicians with access to GenMedPro™, an outstanding tool to help evaluate both gene-drug and drug-drug interactions, pharmacogenetic guideline recommendations, and alternative medication options, as appropriate.
GenMedPro™ can help providers be more informed before prescribing these drugs in older adults if there is additional risk (i.e. increased drug exposure). To learn more about GenMedPro™ or to request a demonstration from our PhD and PharmD experts, please utilize Genomind’s Clinician Portal.
Are You Ready to Upgrade Your Practice with Genomind?
Genomind’s pharmacogenetic testing is the most advanced and comprehensive mental health pharmacogenetic test available. Get access to 24 genes related to mental health, 130+ medications, 10+ conditions, state-of-the-art tools, and 360 degrees of support. Register today.
References
- Lieberman JA 3rd. Managing anticholinergic side effects [published correction appears in Prim Care Companion J Clin Psychiatry. 2012;14(1):PCC.12lcx01362]. Prim Care Companion J Clin Psychiatry. 2004;6(Suppl 2):20-23.
- Merriam-Webster. (n.d.). Anticholinergic. In Merriam-Webster.com dictionary.
- Ghossein N, Kang M, Lakhkar AD. Anticholinergic Medications. [Updated 2021 May 17]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2021 Jan-.
- By the 2019 American Geriatrics Society Beers Criteria® Update Expert Panel. American Geriatrics Society 2019 Updated AGS Beers Criteria® for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc 2019;67(4):674-694.
- Salahudeen MS, Duffull S, & Nishtala PS. Anticholinergic burden quantified by anticholinergic risk scales and adverse outcomes in older people: a systematic review. BMC Geriatrics 2015; 25;15:31.
- Lisibach A, Benelli V, Ceppi MG, et al. Quality of anticholinergic burden scales and their impact on clinical outcomes: a systematic review. Eur J Clin Pharmacol 2021;77(2):147-162.
- Boustani M, Campbell N, Munger S, Maidment I, Fox C. Impact of anticholinergics on the aging brain: a review and practical application. Aging Health. 2008;4:311–320.
- Cebron Lipovec N, Jazbar J, Kos M. Anticholinergic Burden in Children, Adults and Older Adults in Slovenia: A Nationwide Database Study. Sci Rep. 2020;10(1):9337.
- US Food and Drug Administration. Table of Pharmacogenomic Biomarkers in Drug Labeling.
- Hicks JK, Sangkuhl K, Swen JJ, et al. Clinical pharmacogenetics implementation consortium guideline (CPIC) for CYP2D6 and CYP2C19 genotypes and dosing of tricyclic antidepressants: 2016 update. Clin Pharmacol Ther. 2017;102(1):37-44.
Note (title image): The Canadian Deprescribing Network, & Trimble And Currie. (n.d.). [Common Side Effects of Anticholinergic Medications]. WHAT YOU NEED TO KNOW ABOUT ANTICHOLINERGIC MEDICATIONS. https://www.deprescribingnetwork.ca/blog/anticholinergic-medications